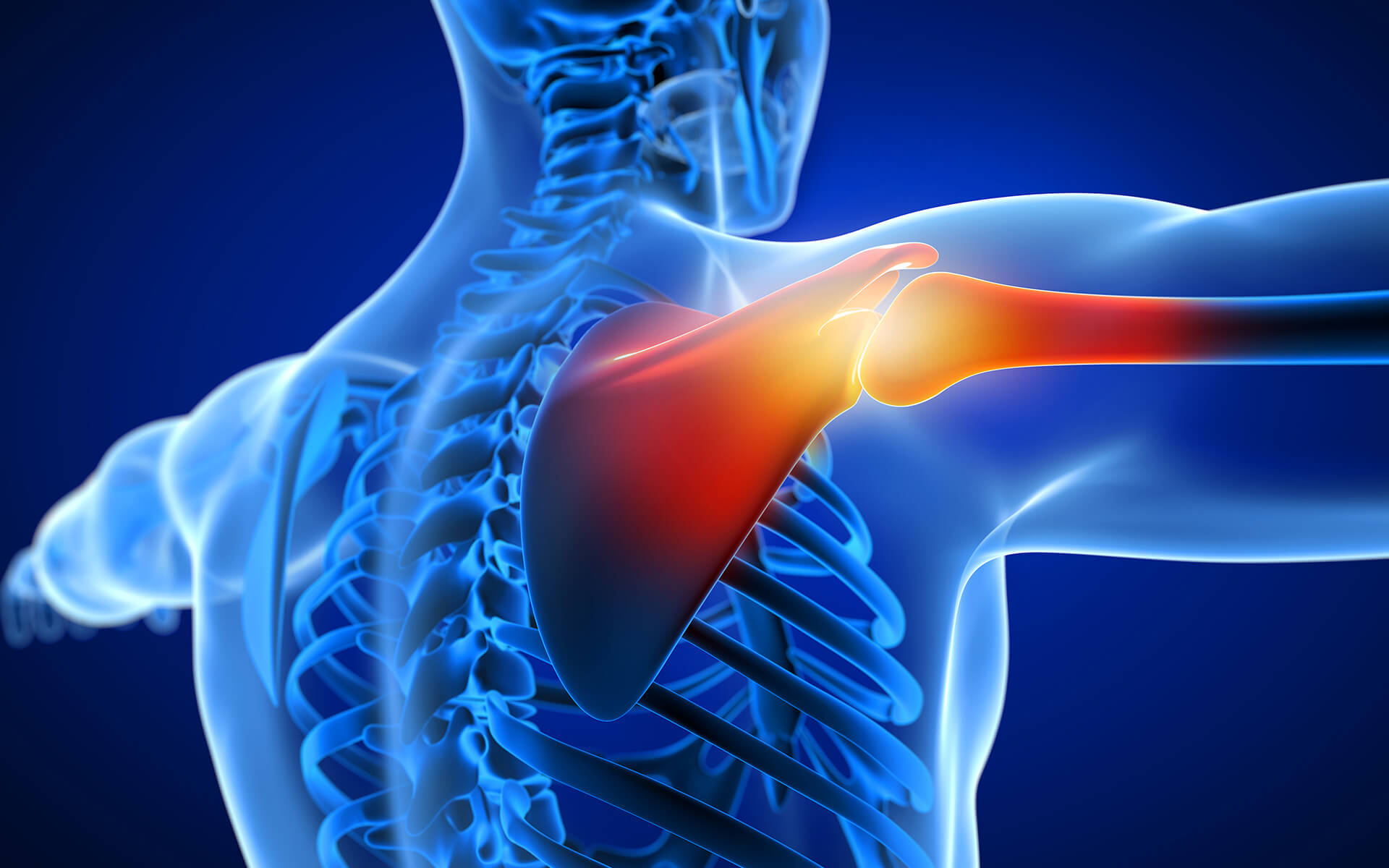
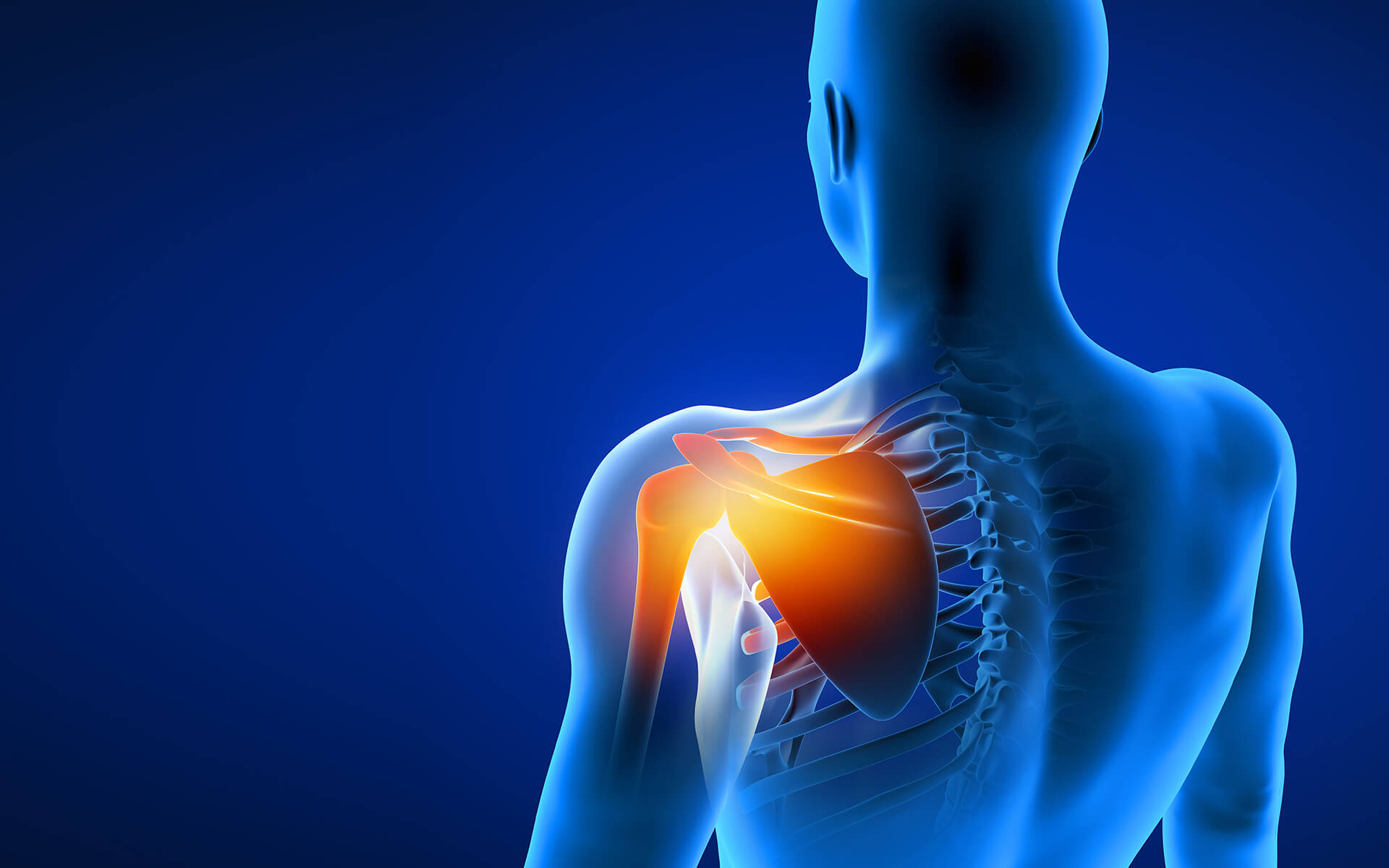
The brachial plexus is a system of five core nerves housed within the shoulder. It controls the back and forth signaling that occurs between the spine and the arms and hands. The greater network of nerves connected to the brachial plexus begins at the nerve root at the top of the neck and flows through the shoulder all the way down to the hands. As part of this network, the brachial plexus is responsible for both movement and sensory signaling (innervation) and activity for the arm, wrist, and hand.
Since the brachial plexus is a network of nerves, injuries that can impact it won’t always occur directly to the shoulder. Neck, back, and spine trauma can also impact the functioning of the brachial plexus.
Minor brachial plexus injuries can cause temporary discomfort, but often heal well, with the patient regaining 90 to 100 percent of the arm’s natural strength and functionality. If the nerve damage is more acute, surgery may be required to treat the impacted nerve(s) and restore as much of the arm’s original mobility and sensation as possible. If you have experienced recent neck or shoulder trauma, watch for signs of a brachial plexus injury and contact the team at the Institute for Advanced Reconstruction for a diagnostic consultation.

-1.jpg)













.jpg)