Graves’ Ophthalmopathy: Your Questions Answered
Graves’ ophthalmopathy, also known as Graves’ eye disease, represents the most frequent non-thyroidal manifestation of Graves’ disease and is characterized by bulging eyes. Ophthalmopathy occurs in 50 percent of Graves’ cases, with severe forms affecting up to 10 percent of cases. Graves’ disease and Graves’ ophthalmopathy are chronic diseases with both physical and psychological symptoms ranging from no manifestations to severe manifestations.
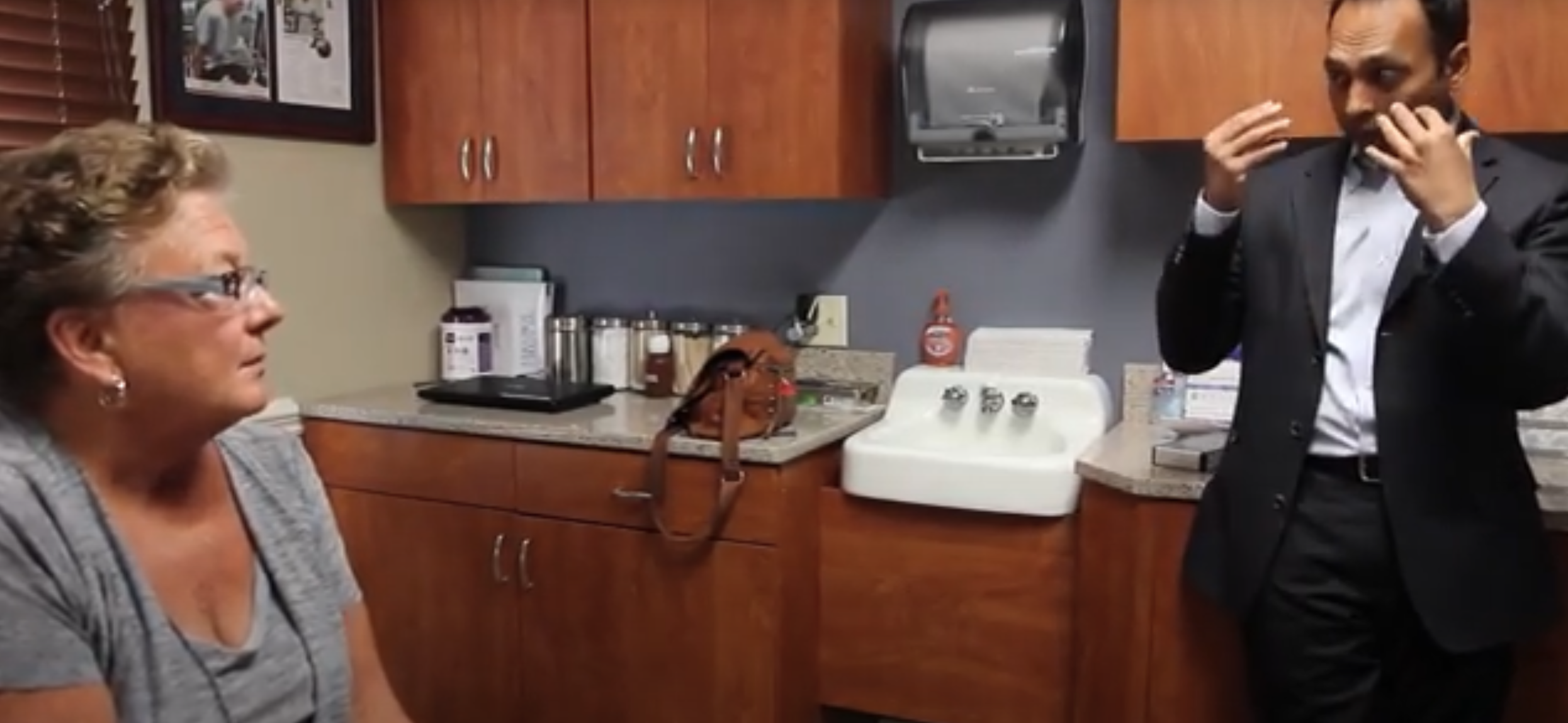
Our Dr. Tushar Patel has extensive experience treating Graves’ Ophthalmopathy with Orbital Decompression Surgery. Recently, Dr. Patel was interviewed on Health Professional Radio and talked about this advanced surgical technique. Listen to the radio interview here or read this excerpt from his interview below:
Host: Graves’ Ophthalmopathy is characterized by bulging eyes, but is it an overactive thyroid-related condition?
Dr. Patel: No. Graves’ disease is the more general medical term causing a hyperactive thyroid. The thyroid just works too aggressively, it’s almost like it is on amphetamines. And what happens is one of the manifestations of patients who have Graves’ disease is that they can have ophthalmopathy, which is a disease-specific to the eyeball itself.
Host: Most people would recognize the term hyperactive thyroid in relation to Graves’ Eye Disease. Can you elaborate a little about why this is?
Dr. Patel: Right. There is a sub-set. So, there are a lot of different reasons to have a hyperactive thyroid, and the most common reason is Graves’ disease. It’s an autoimmune disease, so there are certain markers that can be diagnosed to confirm whether or not a patient has this disease. There’s no cure for Graves’ disease, but it can be controlled.
Host: You mentioned markers to identify patients that are suffering from Graves. Are these genetic markers that can be identified early on in life as opposed to waiting for symptoms?
Dr. Patel: No. There are no genetic markers that I know of as of now, like genes and things like that. But if someone is suspected to have Graves’ disease with the symptoms of a hyperactive thyroid, then there’s a blood test that can be done to confirm the disease.
Host: Talk about a typical patient with this condition I understand that you have treated a woman for Graves’ disease recently. Talk about Mary Ellen Pierce if you would.
Dr. Patel: My patient Mary Ellen Pierce, she’s probably in her late 50’s or maybe early 60’s. She was diagnosed with Graves’ disease a couple of years ago and recently began to have discomfort in her eyes. It started out with just eyes that were really dry, subsequently a little scratchy, leading to the white part of the eye in the morning becoming redder in color from the dryness. As the disease progressed, the eyes started to get more and more irritated. What happened with Mary Ellen is that in Graves’ disease, when the eyes are affected, the eyes have muscles around them, and those muscles are involved in moving the eyeball up and down, side-to-side, so you can look where you want to look. These muscles get infiltrated by fatty tissue, and the disease is responsible for doing this, and then you get swelling around the eye. What happens after that is the eyeball because it’s in the socket that has exact volumes, so if you make that muscle bigger or it gets puffy and enlarges, it pushes the eyeball out of the socket. When that happens, you get the bulging of the eyes that we typically see, and that’s what happened to Mary Ellen. Then, Mary Ellen had surgery for Graves’ disease. There are a couple of ways to treat Graves’ disease. One is to remove the thyroid gland, so that takes care of the disease, or you have to take radioactive iodine, and what that does is suppresses the thyroid, so it does not allow the thyroid to work. But unfortunately, when you do that, whatever happened with the eyes stays that way, or it can progress still for a short period of time. And she was at the point where even though the Graves were not in her system anymore, the eyes were still bulging, irritating and symptomatic.
Host: Is this something that affects men and women equally? Does it affect young adults? Is this something that does not discriminate, or are there some, I guess, for lack of a better term, rules that we can go by when dealing with Graves?
Dr. Patel: It does affect women more than men. There’s about a 2.5 to 3.5 times higher incidence in women than in men. It’s usually middle age to late middle age, so most patients that we see are probably in their 40s or in their 50s. However, my youngest patients that I have had with ophthalmopathy of Graves were in their early 20s.
Host: Briefly talk about the success ratio when it comes to nonsurgical treatments, as you mentioned earlier, radiation, radiated iodine, and the surgeries that you perform within your area of expertise.
Dr. Patel: If we take a hundred patients that are diagnosed with Graves’ disease, only about 20% of them will have eye findings, where the eyes are bulging. The other 80% won’t have any symptoms or manifestations of having issues with the eyes. So then it’s just a thyroid issue and can be treated that way. Of those 20 patients, after they have their iodine and/or thyroid removed, then probably I would say another 40-50% may be okay and will not need anything done for the eyes themselves. That remaining group, the 10%, is in need of some sort of surgical intervention in order to improve the look of the bulging eyes and improve symptoms.
Host: We briefly touched on cancer, and thyroid conditions causing Graves. What about just trauma? Trauma to the eye, a blow, something getting in the eyes, something along the nature that something that is not cancer or something biological, some trauma. Is the treatment going to vary greatly based on nature?
Dr. Patel: It does. That’s a great question because the term “bulging eye” is a very generic term. The majority of patients that have bulging eyes are due to this thyroid, the hyperactivity dysfunction is seen in Graves’ disease. But you can get it from other causes, too. Cancers can be present behind the eyeball or in the socket that can push the eyeball out. So usually, those patients have one side affected and typically get confirming tests like an MRI or CAT Scan to rule out any masses or cancers that may be present. As far as trauma is concerned, for example, if you get punched in the eye or fall on something, again, those usually are one-sided. Also, these are acute injuries, so you’re going to see stigmata like bruising, black and blue, a lot of swelling, and vision changes. There usually is the blood left behind the eyeball that pushes the eyeball out, so we just have to remove the blood to take care of the issue, and that should get better pretty quickly.
Dr. Tushar Patel will be answering questions about Graves’ Disease and Orbital Decompression on a Facebook Live Q&A session on Wednesday, January 24th, at 6 PM EST. Bring your questions, and be sure to tune in for this interactive and informative event! https://www.facebook.com/AdvancedReconstruction/
More information about Graves’ Ophthalmopathy: https://www.advancedreconstruction.com/other-programs/graves/
About the Author: Dr. Tushar Patel
Specializing in reconstructive surgery following traumatic injury and cancer surgery, Dr. Tushar Patel, MD, FACS, is trained in microsurgery and skilled at performing procedures to treat facial deformities. He also developed the DIEP flap technique and muscle-sparing TRAM flap technique, in addition to being an expert in orbital decompression for Graves’ Ophthalmopathy.