Chest Wall Stabilization: What You Need To Know
February is American Heart Month! This month and every month, our practice encourages our patients and friends to live a heart-healthy lifestyle. Did you know that in the US, about 500,000 open heart surgeries are performed each year?
Following heart surgery, some patients experience something called sternal non-union. Sternal nonunion is a term used to describe when the breastbone does not heal properly following heart surgery, which can cause a variety of symptoms. Reconstructive surgeon Dr. Michael Rose performs chest wall stabilization surgery in order to treat sternal non-union.
Q: What are the symptoms of sternal non-union and instability?
Dr. Michael Rose: Usually, the patient notices an uncomfortable clicking or “popping” of the sternal bone, especially when twisting or turning their torso. This is sometimes loud enough to be heard by the patient or even the people around them. Coughing often causes painful mashing of the unhealed edges of the bone against one another. Some people feel like they can’t take a deep breath and often feel short of breath.
Q: What are the causes of sternal non-union and instability?
Dr. Michael Rose: The breastbone is cut right down the middle in most cardiac surgery to access the heart, which is right behind the sternum (breastbone). After cardiac surgery, the cardiac surgeon uses strong wires to knit the two sides of the bone back together in the middle of your chest. Unfortunately, for a small percentage of patients, the bone doesn’t heal together properly, and over time, the wires loosen or break, and the symptoms of sternal instability begin.
Q: What happens if this condition is left untreated?
Dr. Michael Rose: Fortunately, having an unstable sternum rarely causes immediate life-threatening problems. Many people just simply live with an unstable sternum because it doesn’t bother them too much. However, for some people, the symptoms are significant. Some potential problems include infection, bleeding, fractures of the sternum, pain, and shortness of breath. In rare cases, the broken wires can puncture down into the heart cavity or come through the skin. For people with symptoms, treatment is recommended.
Q: How do you treat this condition? How does your treatment differ from other surgical treatments?
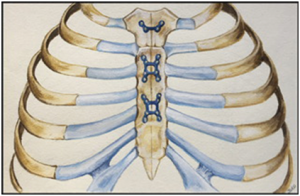
Dr. Michael Rose: The treatment is straightforward: The surgeon will open the same incision that was used for your heart surgery. Directly under the skin is the unhealed bone. The surgeon uses special tools to clean off the fibrous scar tissue that is preventing the bone from healing together and then will bring the edges of the bone together with special clamps. While the bone is clamped tightly together, the reconstructive surgeon places thin titanium plates and screws into the sternum to hold it together permanently. The surgeon then covers the bone and hardware with the pectoral muscles to protect the repaired bone and help with the healing process.
Some surgeons simply re-wire the sternum back together. Some use fancy zip-ties to knit the sternum back together. We have found that the technique of using plates and screws has a higher success rate with fewer complications than these other two methods.
Q: How do you determine if a patient is a candidate for surgery?
Dr. Michael Rose: If they have a non-healed sternum with significant symptoms and are physically able to undergo a 1-hour surgery, then they are a candidate for this surgery.
Q: What does the surgery entail?
Dr. Michael Rose: It’s a one-hour surgery with a one-night stay. The surgery involves the placement of strong plates and screws across the sternum where it has not healed.
Q: What is recovery like?
Dr. Michael Rose: Most patients wake up and immediately feel the difference right in the recovery room. Pain is minimal, and we keep you in the hospital overnight simply for observation. We minimize the use of the arms for 12 weeks while the sternum heals, but after that, you can return to full activity.
“If I had to do it again, I’d do it again because of what it has led me to be able to do and accomplish!”- Robin T., Chest Wall Stabilization Patient of Dr. Rose.