Summarize This Article:
Summarize This Article:

For individuals living with chronic pelvic pain, the impact can be physically, emotionally, and mentally debilitating. If sitting, cycling, or even walking causes sharp, burning pain, you may be suffering from pudendal neuralgia—a condition that’s often misdiagnosed and misunderstood. Our specialists at The Institute for Advanced Reconstruction offer innovative treatments for pudendal neuralgia, designed to relieve pain and restore quality of life.
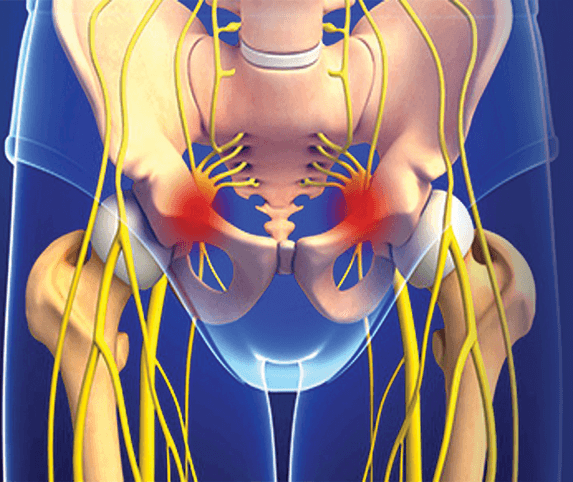
Pudendal neuralgia is a type of chronic pain that arises from irritation or compression of the pudendal nerve. This critical nerve runs through the pelvis and provides sensation to the genitals, anus, and perineum.
Symptoms may include:
These symptoms can severely disrupt daily life, intimacy, and emotional well-being. Unfortunately, because symptoms often overlap with other pelvic disorders, pudendal neuralgia is frequently misdiagnosed.
“It’s not uncommon for patients to be treated for years for unrelated pelvic issues before the nerve problem is uncovered,” explains Hakan Usal, MD, a board-certified plastic and reconstructive surgeon at The Institute. “Our team is highly trained in identifying and treating complex nerve conditions like this.”
Pudendal neuralgia may result from a range of factors, including:
Early, specialized treatment can prevent worsening symptoms and offer a path to lasting relief.
At The Institute, we begin with a comprehensive diagnostic evaluation tailored to each patient’s history and symptoms:
“Accurate diagnosis is the cornerstone of successful treatment,” Dr. Usal emphasizes. “We take the time to investigate every potential cause of pelvic nerve pain.”
Many patients benefit from non-surgical treatments before surgery is considered:
However, if conservative options fail to provide sufficient relief, The Institute offers advanced interventions to address the root cause.
We are at the forefront of interventional pain therapies, offering minimally invasive options that provide meaningful relief:
“These interventions can provide both diagnostic clarity and therapeutic relief,” Dr. Usal explains. “They’re especially helpful for patients who are not yet ready for surgery.”
When other therapies fail, pudendal nerve decompression surgery may be the best option for long-term relief.
When Surgery is Recommended:
What Surgery Involves:
When it comes to treating pudendal neuralgia, few centers offer the depth of expertise found at The Institute.
Why patients trust us:
If you’re living with persistent pelvic pain and believe pudendal neuralgia may be the cause, expert help is available.
Contact Dr. Hakan Usal and the team at The Institute for Advanced Reconstruction to schedule a consultation today. Our specialists are here to help you move forward—pain-free and empowered.